Vitamin D – The Ultimate Guide To The Sunshine Vitamin

Table of Contents
- What is Vitamin D?
- How Do We Get Vitamin D?
- What Does Vitamin D Do for Our Bodies?
- How Much Vitamin D Do We Need?
- What Are the Causes of Vitamin D Deficiency?
- What Are the Symptoms, Signs and Complications of Vitamin D Deficiency?
- What is the Recommended Dose for Vitamin D Supplements?
- What Are the Side Effects and Interactions of Vitamin D Supplements?
- Key Takeaway
- References
What is vitamin D? Discover more about vitamin D, from its sources to the benefits and recommended dose.
More than one in five Australian adults do not get enough vitamin D, which is vital for musculoskeletal health. Vitamin D is structurally different from other types of vitamins. Basically, it’s a steroid hormone produced from cholesterol when your skin is exposed to the sun. Due to this reason, vitamin D is often called “the sunshine vitamin.” Apart from sunlight, some foods also contain vitamin D. But the vitamin D obtained from sunlight and diet is not always adequate.
What is vitamin D?
It is a fat-soluble vitamin. It means that it can dissolve in fats and oils. Your body can store vitamin D for a long time.
It has two forms:
- Vitamin D3 (cholecalciferol)
- Vitamin D2 (ergocalciferol)
Fatty fish, eggs and some other animal foods contain significant amounts of Vitamin D3. Meanwhile, D2 is found in some plants, mushrooms and yeast. Interestingly, vitamin D3 (cholecalciferol) is almost twice as effective at increasing blood levels of vitamin D as vitamin D2.
How do we get vitamin D?
There are three categories of sources of vitamin D.
- Sunlight
- Foods containing vitamin D
- Supplements
Dietary intake is usually quite low because there are only very few foods containing significant amounts of vitamin D. Fatty foods like salmon and other types of fish contain vitamin D. Egg yolks contain small quantities of vitamin D.
Vitamin D deficiency is common, and supplements are widely available to overcome it. They are both safe and effective.
How much sun do we need for healthy bones?
The best source of vitamin D is UVB radiation from the sun. UV radiation levels vary depending on location, time of year, time of day, cloud coverage and the environment.
For most people, adequate vitamin D levels are reached through regular incidental exposure to the sun. When the UV Index is 3 or above (such as during summer), most people maintain adequate vitamin D levels just by spending a few minutes outdoors on most days of the week.
In late autumn and winter in some southern parts of Australia, when the UV Index falls below 3, spend time outdoors in the middle of the day with some skin uncovered. Being physically active (e.g. gardening or going for a brisk walk) also helps boost vitamin D levels.
What does vitamin D do for our bodies?
Vitamin D needs to be active to perform functions in our body. Its active form is calcitriol or 1,25(OH)2D which is obtained by two conversion steps.
Calcitriol attaches with the vitamin D receptors (VDR). These receptors are found in almost every single cell of your body. When calcitriol binds to this receptor, it can turn genes on or off, leading to alterations in your cells. This mechanism of action is similar to how most other steroid hormones work.
Vitamin D performs many functions, particularly bone health. For example, it promotes the absorption of calcium and phosphorus from your gut into the bloodstream. In addition to increasing bone strength, it also plays a role in other areas of health, such as immune functions and protection against cancer. It strengthens the brain and improves your mood.
How much vitamin D do we need?
Vitamin D requirement varies with age, sun exposure, dietary habits, latitude, season, ethnicity.
Assuming no or minimal sunlight exposure, the recommended daily adequate intake (AI) of vitamin D in Australia is 5 micrograms (200 IU) for children, adolescents and adults aged 19–50 years, 10 micrograms (400 IU) for adults aged 51–70 years, and 15 micrograms (600 IU) for adults over 70 years of age.
What are the causes of vitamin D deficiency?
There can be many reasons for vitamin D deficiency. The main reasons include:
- Not getting enough vitamin D in your diet.
- Malabsorption problems or gastrointestinal diseases
- Insufficient exposure to sunlight
- Inefficient production in the skin
- Kidney diseases
- Liver diseases
- Use of medicines interfering with your body’s ability to convert or absorb vitamin D
What are the symptoms, signs and complications of vitamin D deficiency?
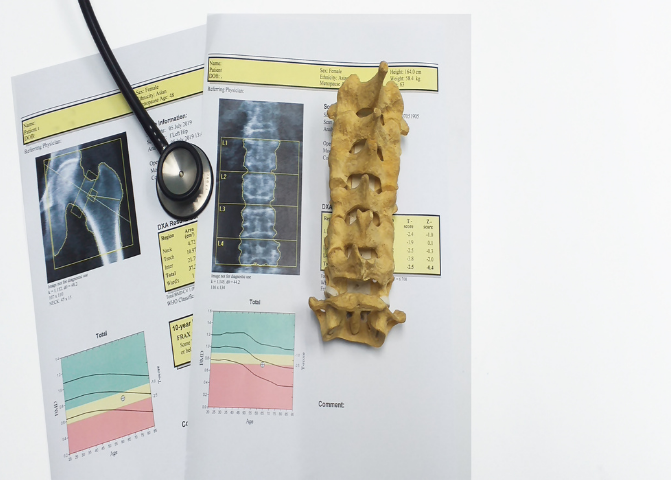
Vitamin D deficiency can cause osteomalacia and rickets (softening of the bones) in children and contribute to osteoporosis and fragility fractures
Rickets manifests itself as incorrect growth patterns, weak muscles, bone pain, and joint deformities. Though this is rare, it can occur with severe vitamin D deficiency in children.
Signs and symptoms of vitamin D deficiency are not quite obvious in young adults. These signs and symptoms include:
- Bone pain
- Muscle weakness
- Muscle aches
- Cramps
- Mood disturbances
Low blood levels of the vitamin D in the blood for a long time can cause:
- Increased risk of cardiovascular diseases
- Cognitive impairment in adults
- Osteoporosis
- Osteomalacia
- Severe asthma in children
- Cancer
What is the recommended dose for vitamin D supplements?
In Australia, guidelines recommend vitamin D3supplementation at 25–50 micrograms (1000–2000 IU) per day for people with mild vitamin D deficiency.
For moderate to severe deficiency, vitamin D3supplementation is recommended at 75–125 micrograms (3000–5000 IU) per day for 6–12 weeks, or 1250 micrograms (50,000 IU) once a month for 3–6 months.
All patients are recommended to maintain a total daily calcium intake of 1300 mg.
Vitamin D supplementation for older people in care facilities is recommended, to reduce the rate of falls. Vitamin D supplementation may reduce the risk of falls by improving muscle strength and functioning.
What are the side effects and interactions of vitamin D supplements?
Vitamin D is generally safe with other medications and supplements. Side effects of vitamin D supplements are rare and occur only when they are taken in too much quantity. Mostly, these side effects are mild. They include:
- Sleepiness
- Loss of appetite
- Headache
- Nausea
- Vomiting
- Dry mouth
- Metallic taste
- Fatigue
Vitamin D can interact with the following substances:
- Aluminium
- Calcipotriene
- Digoxin
- Diltiazem
- Water pills (Thiazide diuretics)
- Verapamil
- Cimetidine
- Heparin
- Low molecular weight heparins (LMWHS)
It’s important to discuss the needs, risks and benefits of vitamin D supplementation with your doctor.
Key Takeaway
Vitamin D is a fat-soluble vitamin that performs many functions such as strengthening bones, reducing depression and preventing the risk of many diseases. Its deficiency is quite common and can be easily treated by supplements and lifestyle changes. It’s important to discuss your general health with your GP and the indications, benefits and risks of supplementation.
References
- Haines, S. T., & Park, S. K. (2012). Vitamin D supplementation: what’s known, what to do, and what’s needed. Pharmacotherapy, 32(4), 354–382. https://doi.org/10.1002/phar.1037
- Nair, R., & Maseeh, A. (2012). Vitamin D: The “sunshine” vitamin. Journal of pharmacology & pharmacotherapeutics, 3(2), 118–126. https://doi.org/10.4103/0976-500X.95506
- Pramyothin, P., & Holick, M. F. (2012). Vitamin D supplementation: guidelines and evidence for subclinical deficiency. Current opinion in gastroenterology, 28(2), 139–150. https://doi.org/10.1097/MOG.0b013e32835004dc
- Gani, L. U., & How, C. H. (2015). PILL Series. Vitamin D deficiency. Singapore medical journal, 56(8), 433–437. https://doi.org/10.11622/smedj.2015119
- Gani, L. U., & How, C. H. (2015). PILL Series. Vitamin D deficiency. Singapore medical journal, 56(8), 433–437. https://doi.org/10.11622/smedj.2015119
- Matyjaszek-Matuszek, B., Lenart-Lipińska, M., & Woźniakowska, E. (2015). Clinical implications of vitamin D deficiency. Przeglad menopauzalny = Menopause review, 14(2), 75–81. https://doi.org/10.5114/pm.2015.52149
- Sahota O. (2014). Understanding vitamin D deficiency. Age and ageing, 43(5), 589–591. https://doi.org/10.1093/ageing/afu104
- Lamberg-Allardt C. (2006). Vitamin D in foods and as supplements. Progress in biophysics and molecular biology, 92(1), 33–38. https://doi.org/10.1016/j.pbiomolbio.2006.02.017
Join the Medmate Community!
Receive free expert health advice from Australian doctors and health advisors. Join the Medmate community now - just what the doctor ordered.
Health Information I Medication Education & Tips I Patient Stories & Videos.