The Evolution of the National Doctor: Transforming Australian Healthcare Through Virtual Health
by Dr Ganesh Naidoo,Co-Founder, CEO, and Medical Director @ Medmate
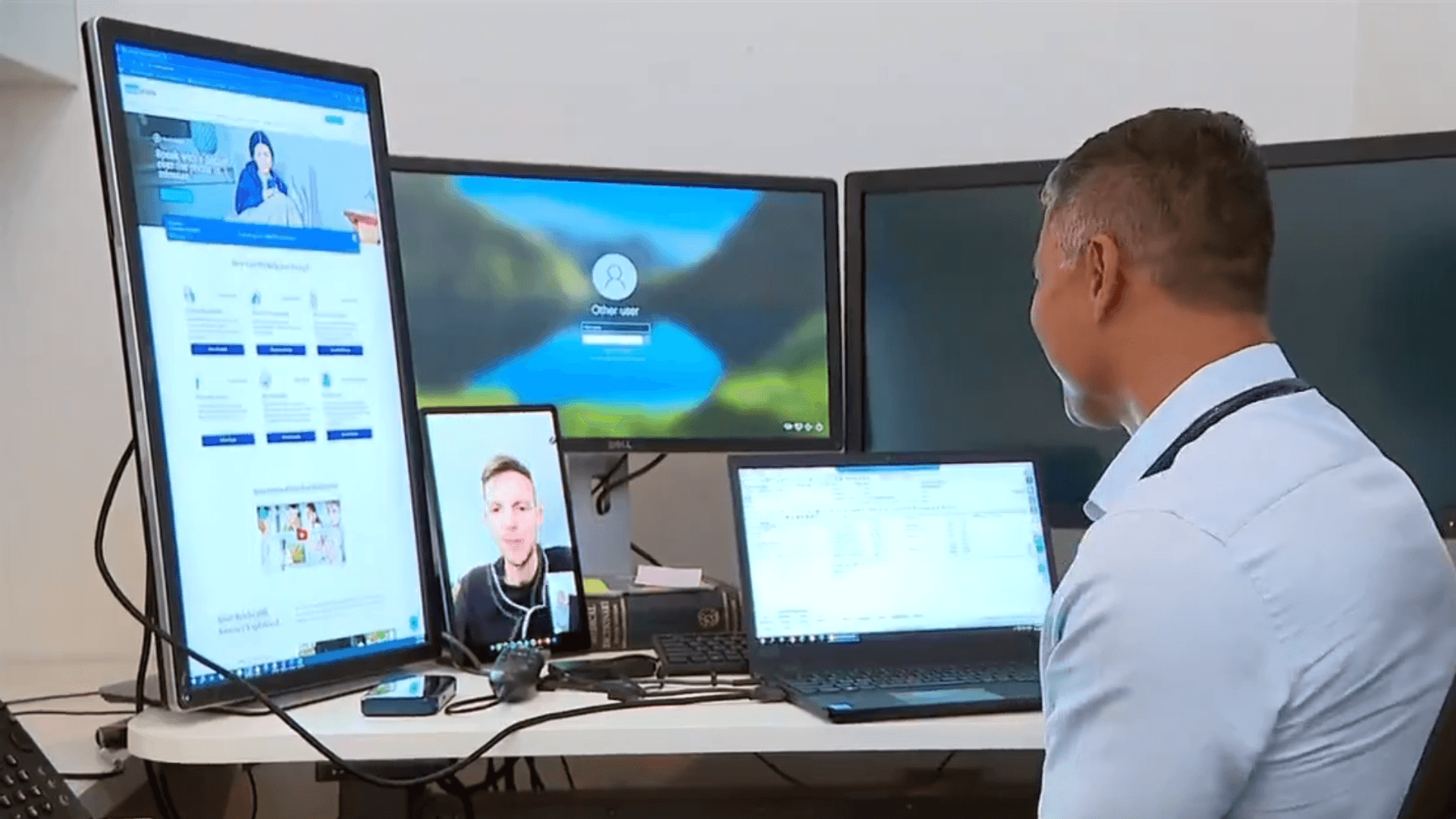
Imagine this: in a single morning, I’m consulting with a stressed-out office worker on Collins St Melbourne, then a miner battling long shifts in Western Australia, and moments later, a parent in Far North Queensland worried about their child in the swelter of the wet season. I’m not hopping on planes or driving across the country—I’m doing it all from my clinic, through the power of telehealth. As a hybrid doctor, splitting my time between face-to-face and virtual consultations, I’ve witnessed the dawn of a new era in Australian healthcare. The rise of the “national doctor” has shattered the boundaries of the traditional local doctor, and the impact is nothing short of revolutionary. Let me take you into my world, where technology, empathy, and medical expertise come together to bridge distances and transform lives, one virtual visit at a time.
Being a national doctor is a dramatic departure from the traditional role of a local doctor. It requires a new set of skills: the ability to understand people’s lives in diverse geographies, navigate local healthcare environments thousands of kilometers away, and address the frustrations of those in remote areas with far less access to care than their inner-city counterparts. I hear firsthand the stark disparities in healthcare access—patients in rural and remote regions often face barriers that metro patients simply don’t face. This was certainly not something we were trained for in medical school, where the focus was on in-person consultations and physical examinations – a 19th century view of the world.
Consulting via telehealth is an art form, one that demands the highest level of communication skills. Only the very best doctors can excel in this space. Over a phone call, I must “hear” how unwell someone is—picking up on subtle cues in their voice, sensing anxiety or a flat affect through tone alone. On a video call, I might assess a sick child, interpreting what I see and hear without the ability to reach through the screen to physically examine them. It’s a unique challenge, but also a profound opportunity. Medicine has always been an art, a delicate balance of probabilities informed by history-taking, physical examination, and investigation results. Drawing from thousands of patient interactions, we make data-driven decisions, forming conclusions, differential diagnoses, and management plans through pattern recognition—often described by doctors as a “sixth sense.” Telehealth elevates this art to another level.
In some ways, telehealth reduces the dataset we work with—I can’t touch a patient to exam a knee or palpate an abdomen. But in other ways, it expands it. Through a video call, I see patients in their home environment, gaining insights into their living conditions and daily realities. They’re often more open in this safe, discreet, and comfortable space, sharing details they might not in a clinical setting. This added context becomes a powerful tool in forming a care plan.
Looking ahead, the evolution of telehealth technology and AI promises to further revolutionize healthcare access. Advanced AI algorithms are being developed to assist doctors in triaging patients, analyzing symptoms, and even predicting potential health issues before they become critical, all through virtual platforms. AI-driven diagnostic tools can process voice patterns or video feeds to detect early signs of conditions like respiratory distress or mental health challenges, enhancing the accuracy of telehealth consultations. Meanwhile, telehealth platforms are integrating with wearable devices to provide real-time data on patients’ vital signs, enabling more precise monitoring and personalized care, especially for those in remote areas. These advancements will not only bridge the gap in access but also empower patients with tools to manage their health proactively, ensuring that high-quality care reaches even the most isolated communities with greater efficiency and impact.
As a national doctor, I must think critically about the resources available to each patient in their local environment. What risks do they face? What safety nets are in place if their local options fail? How can I ensure they’re supported, no matter where they are? It’s extraordinarily complex—requiring not just medical expertise, but also technology capabilty, common sense, and an understanding of local healthcare systems. Yet, it’s also deeply fulfilling. Leveraging virtual health, I can provide care to anyone, regardless of who they are or where they come from, breaking down the geographic barriers that once defined medical practice.
The evolution from a local doctor to a national doctor is a testament to how technology is reshaping healthcare in Australia. It’s a privilege to be part of this transformation, using my skills to reach patients in every corner of the country, ensuring they receive the care they need. The national doctor is here to stay, and I’m proud to be at the forefront of this new era in medicine.
Join the Medmate Community!
Receive free expert health advice from Australian doctors and health advisors. Join the Medmate community now - just what the doctor ordered.
Health Information I Medication Education & Tips I Patient Stories & Videos.
